By: Luke Hansen, Arcadia
This guest post is contributed by Arcadia, a leading data platform for healthcare organizations, helping providers harness data for better patient outcomes.
Patients want to feel like more than just another name on the sign-in sheet at their physician’s office—they want to feel known as people. This is especially true of patients facing chronic conditions who need ongoing care and engagement. Provider trust is critical to these, and personalized care earns that trust.
Healthcare trends suggest that combining high-tech solutions with a personalized touch is essential for meeting patient expectations, lowering costs, and improving overall outcomes. In other words, personalized care drives optimized patient experiences.
This article uncovers the specific ways that personalized care improves the patient experience and why this approach is essential for patients with complex needs.
Reduces Risk of Poor Outcomes
A one-size-fits-all care approach not only fails to meet patients’ expectations but can also lead to poorer health outcomes. Research shows that five of the top 10 leading causes of death in the U.S. are (or are strongly associated with) preventable, treatable chronic diseases.
Successful management cannot occur without longitudinal care relationships. Health systems can support better health outcomes by providing whole-person care, which involves considering all of the factors that impact a patient’s health status, including their health risks, preferences, and social context. This inclusive consideration will keep patients engaged in their care journey.
As such, personalized care enables care teams to:
- Proactively identify symptoms. By looking at a patient’s holistic, self-reported needs, providers can detect health issues early and deliver timely care before complications arise.
- Adapt care plans to the social context. Providers can modify patient outreach and care plans based on the non-medical factors influencing a patient’s health.
- Individualizing communication. Care teams can use personalized communications to engage patients in their own care and improve adherence to treatment plans.
For example, consider a patient living with complex diabetes who begins experiencing early symptoms of a diabetic foot ulcer (DFU). With a personalized care plan in place, the patient’s care team can identify these symptoms early and reach out with clear, empathetic guidance on how to manage their symptoms. As a result, the patient could prevent severe complications that would lead to hospitalization and gain deeper trust in their care team.
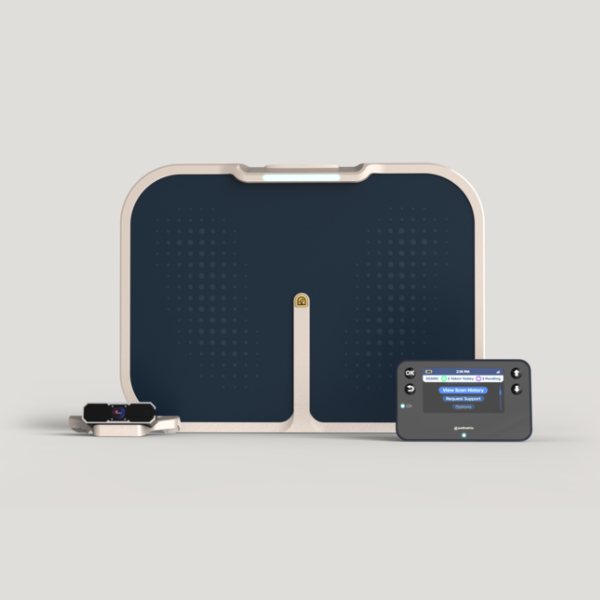
As Arcadia explains, chronic care support software is a vital tool in delivering high-quality care. These tools provide the capabilities for effective data management and analytics, allowing health organizations to identify patients at risk so care teams can intervene and improve the patient’s outcome. With the right infrastructure and capabilities, providers can zero in on patients’ individual needs.
Enhances Care Coordination
Data drives personalized care by enabling different members of a patient’s care team to view holistic medical histories. As a result, patients experience smoother care transitions and receive more timely and effective treatments.
For instance, the patient living with complex diabetes in our earlier example might see a primary care physician (PCP), a podiatrist, and an endocrinologist. Fragmented clinical data across these providers is frustrating for the patient and everyone on the care team. Under a personalized approach, all parties will analyze data about the patient’s prior visits to align their treatment plans.
Health systems looking to strengthen care coordination should:
- Maintain a unified view of each patient’s care journey. Care teams must look at a wide range of data, including medical histories, patient-generated data, and social determinants of health (SDoH), for a holistic view of patient needs. Centralized data systems are critical to ensure no patient data slips through the cracks.
- Strengthen patient communications and handoff procedures. Clear communication allows you to answer patients’ questions, make discharge or at-home recovery instructions easy to follow, and ensure follow-through on treatment plans.
- Implement performance improvement initiatives that prioritize care quality. When health teams make a dedicated effort to enhance care quality, patients receive consistent and effective treatment across various providers. For health organizations, this may involve setting clear benchmarks and tracking their progress toward care delivery goals.
When providers, payors, and other members of a healthcare delivery system work together seamlessly, patients feel more known and understood and ultimately reap the benefits.
Drives Patient Engagement
Robust data and an effective warehouse for organizing usable data points provide a comprehensive view of individual patients within a population. As a result, care teams can deliver precise outreach that aligns with each patient’s needs and preferences, ultimately increasing patient engagement.
By enabling tailored communications and treatment plans, personalized care supports:
- Stronger patient-provider relationships. Personalization reinforces the sense of connection and trust between patients and their care teams, making patients feel seen.
- Increased adherence to medication and care plans. When patients understand their care plans, they’re more likely to become active in their care, leading to higher treatment adherence and better outcomes.
- More engaged in necessary care. Engaged patients are more enthusiastic about addressing their care, leading to more participation in preventive care and fewer appointment no-shows. Additionally, patients who feel more ownership and control over their care journey feel more confident in decision-making.
Beyond individual outcomes, heightened patient engagement also reduces complications and emergency events, lowering the overall cost of care. Additionally, high engagement rates can positively influence healthcare performance indicators, such as readmission rates and patient satisfaction metrics.
Personalized Care: A New Standard for Chronic Condition Management
The evolution of data and technology is driving a more personalized approach to healthcare. However, personalized care isn’t limited to patient experiences in medical practices or adherence to treatment plans after hospital discharge.
Every team across the care continuum can implement personalized care practices and drive patient experiences that improve outcomes. By combining empathetic support and tech-enabled tools, health teams can truly meet patients where they are.