By Candice Bucknor, Manager, Clinical Services
From Access to Outcomes: What Comes After the First Appointment
Our recent blog, “Advancing Equity in Wound Care: Investing in Early Detection to Improve Outcomes”, explored barriers that prevent patients in underserved communities from receiving timely wound care. Delayed treatment leads to both clinical complications and rising costs, highlighting the urgent need to make early detection tools and treatments more accessible, especially for high-risk patients. But what happens after a patient gains access to these services? Equity isn’t just about access—it’s about what happens next.
This next phase of the conversation shifts the focus from who receives care to how that care is delivered, and why outcomes still fall short even when access exists. Addressing these gaps means confronting the deeper structural issues within our healthcare system—the ones that shape experiences, limit options, and ultimately determine results. By addressing these structural inequities that persist within healthcare delivery, we can build a more accountable, inclusive, and effective wound care system that delivers consistent outcomes for all patients.
The Structural Realities Undermining Wound Care Equity
While many efforts concentrate on improving access to healthcare, fewer address what occurs after that access is granted. Too often, patients still face inadequate treatment due to underlying system flaws.
- Workforce Gaps in High-Need Areas: There’s a critical shortage of wound care specialists in many rural and low-income urban communities. As a result, patients often face long waits, travel long distances, or receive care from providers who aren’t trained to manage complex wounds. This shortage not only jeopardizes the quality of care patients receive but also places an immense burden on already vulnerable populations.
- Unequal Treatment Due to Implicit Bias and Discrimination: Implicit bias can shape diagnosis and care plans, contributing to delayed referrals, mismanaged treatment, or fewer limb-preserving interventions for patients of color. A study published in the National Library of Medicine reveals that racial and ethnic minorities receive lower-quality care due to implicit biases within the healthcare system. These biases perpetuate disparities and undermine trust, leading to worse health outcomes for marginalized groups.
- Language and Cultural Barriers: Language differences and cultural misunderstandings can hinder effective communication, causing patients to struggle in expressing their needs or trusting the care they receive. Without culturally competent care, critical details can be overlooked, negatively impacting health outcomes.
- Fragmented Care Models: Wound care often requires coordination between specialists, primary care providers, and home health teams. When systems don’t support seamless collaboration, care becomes reactive instead of preventive, and patients can fall through the cracks.
When these barriers are left unaddressed, the consequences extend far beyond statistics. They show up in preventable complications, emotional distress, and long-term financial strain for patients, families, and communities alike. The ripple effect reaches across the healthcare system, deepening inequities and driving unsustainable costs.
The Cost of an Unequal System
Even with early detection tools available, an inequitable system can still produce negative outcomes—impacting not just individual patients, but the healthcare system as a whole.
Without strong follow-up care and specialist input, early-stage wounds may still escalate into irreversible complications, leading to higher rates of preventable amputations. When wound complications progress, they often result in permanent disabilities that require costly ongoing care, rehabilitation, and support services — placing a significant financial burden on patients.
The economic impact extends far beyond individual patients. Preventable complications drive long-term disability, lost income, caregiver strain, and rising public healthcare costs. Technology alone cannot solve these challenges. To truly advance equity in wound care—including wound-related complications — we must rebuild and strengthen the systems that not only connect patients to care, but also support them throughout their healing journey.
What a Truly Equitable System Looks Like
Solving the root causes of inequity in wound care means more than expanding services. It requires intentional investment in people, infrastructure, and accountability.
- Expand and Equip the Workforce: In order to create an equitable wound care system, there must be a robust and well-distributed workforce, particularly in underserved regions where access to specialists remains limited. Providers trained in cultural competency and trauma-informed care deliver services that better reflect and respond to diverse patient needs.
- Build Accountability into Policy: Policies that prioritize accountability help drive real change. Tracking outcomes like amputation rates and healing success by race, geography, and insurance status reveals where disparities persist and allows targeted interventions. Tying reimbursement to quality metrics, rather than service volume, strengthens the system’s focus on meaningful outcomes.
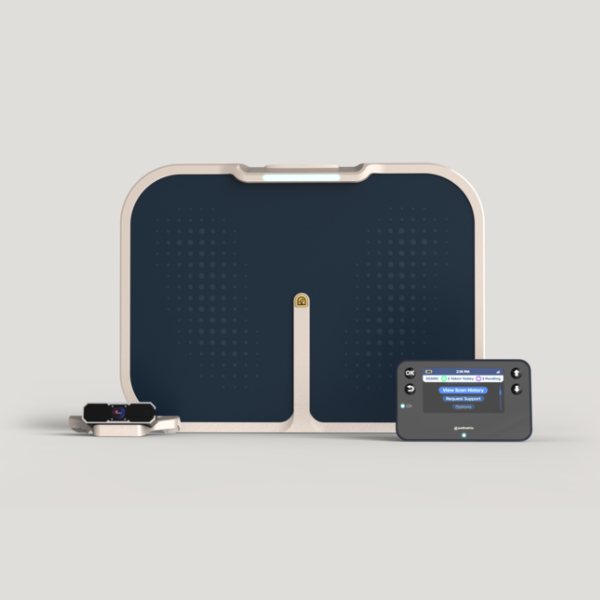
- Center Innovation on Affordability and Reach: Expanding access to wound care means rethinking where and how it happens. Prioritizing low-cost, easy-to-use technologies can bring early detection and treatment into homes, rural clinics, and underserved communities. Telemedicine and mobile health units are key to reaching patients where they are, especially those with limited access to in-person care. Recent insights from Podimetrics’ article about key lessons in creating a positive patient experience for a remote foot health program highlight how designing technologies around ease of use and continuous support can dramatically improve outcomes, particularly for patients managing complex conditions like diabetic foot ulcers. While Podimetrics focuses specifically on early detection and remote monitoring to help prevent complications like diabetic foot ulcers, many of the principles we’ve applied—such as ease of use, continuous support, and proactive care—are relevant across the wound care continuum. The strategies we’ve used to support early detection and patient engagement—like simplifying technology and offering ongoing support—can also help improve care access, reduce disparities, and ensure more patients get the timely, coordinated care they need.
- Close the Loop on Care: Closing the loop on care is critical for preventing patients from falling through the cracks. Systems that support smooth transitions between clinics, specialists, and home health teams keep patients engaged across every phase of their healing journey. Investing in digital infrastructure and patient navigators strengthens continuity of care and reduces the risk of complications caused by fragmented services.
These strategies illustrate what a truly equitable wound care system can look like: one that expands access, closes gaps, and delivers healing with consistency and compassion. With collective action, we can build systems that truly serve underserved communities and ensure that every patient, no matter where they live or what they earn, has a fair chance at healing.
What It Takes to Deliver on Equity
True equity in wound care isn’t just about access—it’s about transforming how care is delivered and supported. When care teams are connected, patients are empowered, and systems are built with compassion and accountability, better outcomes follow. At Podimetrics, we’re dedicated to preventing diabetic foot complications before they begin, helping healthcare organizations close critical gaps in care. Together, we can build a system where every patient has a fair and supported path to healing.
Learn how Podimetrics is helping prevent complications before they start.