By Gary Rothenberg, DPM, CDCES, CWS, Director of Medical Affairs at Podimetrics
Throughout my 25 years of practice, I have utilized various skin substitutes to aid in the healing of diabetic foot ulcers (DFUs). As a student of evidence-based medicine who grew up in the wound care space, the work of Peter Sheehan was foundational. His publication titled “Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial,” gave practitioners not only the ability to implement advanced wound modalities like skin substitutes, but also the charge to use them when a patient’s wound was not trending towards healing at 4 weeks. Since the late 1990s, the availability of novel skin substitutes, evidence-based research on their use, and access to reimbursement have been game-changing in how we approach DFU care.
The Rise of Skin Substitutes in DFU Care
Skin substitutes are bioengineered products designed to promote wound healing by replacing or supporting damaged tissue. They act as scaffolds of extracellular matrix, donating growth factors that are missing in chronic wounds. Depending on the product, they may be derived from human cells, animal tissue, or entirely synthetic materials. Before the development of skin substitutes, options for healing DFUs were limited to traditional secondary wound healing or autologous skin grafting, which involves taking skin from one anatomic area of the same patient to cover another. While potentially successful, traditional operative skin grafting is often associated with high procedural costs, donor site pain, and increased risks for an already high-risk patient population.
Over the past several decades, the benefits of using skin substitutes have become increasingly evident, including enhanced healing rates, decreased risk of amputation, and reduced wound recurrence. With products like Apligraf and Dermagraft paving the way, there has been an explosion of wound care products designed to help heal these recalcitrant wounds. The market continues to grow and expand with emerging sources that I would have never dreamed of, like Icelandic fish skin, which has demonstrated quicker closure and more robust tissue regeneration when applied to DFUs. Of course, there are still limitations in using skin substitutes, including access and awareness, judicious and appropriate patient selection, and the affordability of potentially high patient copays.
There is clearly no shortage of DFU cases, and no hesitation among health care providers to use skin substitutes. In 2024, biologic skin substitutes represented over 54% of the diabetic foot ulcer biologics market. Products like Apligraf and Dermagraft collectively accounted for the majority of skin substitute episodes in large data surveys. According to a four-year analysis of Medicare patients, the average reimbursement per episode ranged from $1,435 for some acellular matrices to $14,424 for advanced cellular products.
A Booming Market with Unintended Consequences
Recently, The New York Times called attention to the overuse of skin substitutes, noting how Medicare spending on skin substitutes has skyrocketed, exceeding $10 billion in 2024. This outpaced Medicare expenditures for ambulance services, anesthesia, and even CT scans. Since 2023, over 100 new and expensive skin substitute products have flooded the market. Many have been introduced with minimal evidence-based research supporting their use and little oversight, enabling manufacturers to set extremely high prices for these seemingly “me too” products.
Unfortunately, in some cases, physicians can purchase these products at discounts and bill Medicare at the full price, pocketing the difference. This creates incentive to use these products when potentially unnecessary, contributing to substantial waste and abuse. As of July 2025, Medicare announced a dramatic reimbursement reduction for these products, instituting a standardized payment cap of $806 per square inch. This is a significant drop from previous reimbursement levels and is intended to curb profiteering and unnecessary use.
Rebalancing the Future of Diabetic Foot Care
While I am thankful that skin substitutes and other advanced modalities exist to help heal DFUs, I often think about how different care would look if we didn’t need them so often. It may sound over the top, but imagine a world where we didn’t need as many fancy goops, gels, or even fish skin. Are we truly prioritizing prevention of DFUs over healing them? Both the literature and real-world experience suggest we’re not. According to Bus and colleagues, 75% of DFU are preventable, highlighting a critical need to redirect efforts on prevention in both clinical care and research. Refocusing our approach means emphasizing proven prevention strategies for high-risk patients with diabetes including foot education, routine care, appropriate shoes and inserts, and foot temperature monitoring.
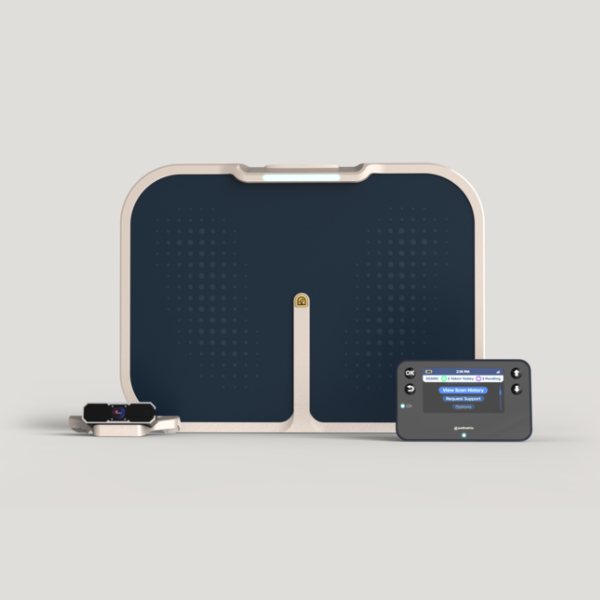
The primary goal is to prevent a patient’s first diabetic foot ulcer (DFU), but for high-risk patients with diabetes, secondary prevention is crucial due to their high recidivism rates after a previous DFU or partial foot amputation. In a study involving high-risk Medicaid members, Podimetrics collaborated with a health plan to implement timely interventions aimed at preventing complications before they happen. Over the span of twelve months, amputations were reduced by over 50%, and even more impressively, the use of skin substitutes decreased by more than 60%. These reductions, along with fewer emergency room visits and shorter hospital stays, led to 20% cost savings, translating to $7,200 saved per member per year.
This highlights the importance of proactive diabetic foot care and emphasizes the need for a preventive approach. Preventing diabetic foot ulcers not only improves health outcomes but also reduces costs, making it a combination that deserves greater attention. While skin substitutes play an important role in treatment, the rising costs and questionable value of many newer products raise concerns about overuse. The truth is, the tools we need to prevent DFUs already exist and have been proven to reduce complications and lower costs. The goal isn’t to replace skin substitutes, but to rebalance our approach. By prioritizing prevention and using advanced therapies more selectively, we can help patients avoid DFUs in the first place rather than relying on expensive solutions after the fact.
Want to take a deeper dive?
Download our study to explore how one plan reduced the cost of skin substitutes by more than 60% with Podimetrics’ virtual care solution.