Diabetes affects people from all backgrounds and all walks of life, so communication and understanding between providers and patients is essential for achieving the best outcomes. Cultural differences can shape how care and treatment are accessed or understood, which may, in some cases, increase the risk of foot complications like ulcers and diabetic amputations.
For example, some individuals within Asian cultures may perceive insulin use as a social obstacle that could impact marriage prospects, leading some to refuse this diabetes treatment, according to a study in Diabetes Spectrum. Language barriers may be a hurdle to diabetes foot care, as they can lead to gaps in care among minority groups who may not understand the guidance for preventing ulceration.
Acknowledging these and other cultural barriers in diabetic foot care may increase patient engagement and connect people with the compassionate care they need to avoid ulcers and amputation. Here’s a closer look at the barriers providers and payors face, along with suggestions that may lead to greater health equity in diabetes.
How Do Cultural Differences Affect Outcomes in Diabetes?
Family, religion, and social expectations are some of the many cultural factors that may affect diabetes outcomes across a spectrum of ethnic and racial minority groups. In the U.S., diabetes rates are two to six times higher among non-White populations, including African Americans, Native Americans, Hispanics/Latinos, and Asians, reports Clinical Diabetes. JAMA Network Open says that these same minority groups also have a several-fold greater risk of diabetic amputation than Whites. Understanding how certain cultural values shape healthcare perspectives allows providers to engage more effectively and respectfully.
Here’s a breakdown of how cultural differences affect the diabetic foot care and amputation risk.
Family
Individuals within some cultures, such as Hispanic communities, may consult with their families before initiating certain medical treatments—a concept known as familismo. Familismo refers to respecting and being loyal to the extended family. In these contexts, the health and well-being of the family unit are often deeply interconnected with individual healthcare decisions.
According to the study in Diabetes Spectrum, as mentioned earlier, familismo can influence health decisions, sometimes leading to challenges with blood sugar control or medication adherence, which may contribute to outcomes like foot ulcers and amputation.
Social Factors
Diabetes management—including diabetic foot care—is viewed as a major inconvenience in some cultures, as it equates to less time for work and social activities. In some communities, the stigma around diabetes or the visibility of treatment tools like syringes may discourage individuals from seeking care or administering medications publicly. In some cultures, women are often the caregivers and believe in putting the needs of their children and spouses before their own. These social factors may sometimes lead individuals at risk for ulcers to deprioritize their foot health and treatment regimens.
Language
A study in Diabetes Care reports that language barriers affect diabetes outcomes and amputation in several ways, including decreased access to health care, poor treatment adherence, and higher mortality. Language barriers can contribute to challenges such as treatment delays or miscommunication about care plans, emphasizing the need for clear and accessible communication. Diabetes Spectrum adds that the quality of diabetes care is reduced even when interpreters are available due to cultural differences in body language, gestures, and the meanings of words.
Health Literacy
Health literacy is generally defined as the degree to which people can obtain, process, and understand basic health information needed to make informed health decisions. Evidence suggests that low health literacy is linked to higher rates of hospitalization and poor disease outcomes, including diabetic foot ulcers and amputation. Daily foot inspections, toenail trimming, and regular bathing are some components of diabetic foot care that may be neglected due to low health literacy.
Religion and Spirituality
Some individuals in certain cultural groups, including some Hispanics and African Americans, may incorporate prayer as part of their coping strategies and view diabetes as a spiritual test. These ethnic groups may avoid or delay diabetes treatment in favor of prayer. Similarly, during Ramadan, some Muslims may avoid medication while fasting, adhering to religious guidelines.
These deeply rooted practices reflect significant cultural and personal values, though they may occasionally create challenges in maintaining stable blood sugar levels or preventing complications like diabetic foot ulcers.
How Can Providers Address Cultural Barriers in Diabetic Foot Care?
Cultural barriers in diabetic foot care can feel overwhelming for both healthcare providers and payors. However, adopting culturally sensitive strategies can help bridge these gaps. By collaborating closely with patients, providers can navigate challenges respectfully, aligning care strategies with patients’ beliefs while promoting effective diabetes management.
Here are some strategies providers can use to address cultural considerations in diabetic foot care and foster stronger patient relationships:
- Review how social determinants of health (SDoH) and health equity affect diabetes. SDoH are non-medical factors that can impact a person’s health, such as social and economic conditions, education, and access to healthcare. Becoming familiar with SDoH can help providers identify underserved populations at the highest risk for diabetic amputation and act accordingly.
- Learn about the religious practices of the populations being served. Religious beliefs and values vary among different cultures, and providers should address them before starting care programs and medications.
- Understand the role and importance of family within a specific culture or community. In some cultures, such as Hispanics and Latinos, for example, entire families may prefer to be consulted or involved in diabetes treatment to reduce the risk of diabetic amputation.
- Explore alternative treatment options for cultures with negative views about medication. Treatments can be personalized for cultures that are likely to refuse insulin or other medications due to social and religious factors.
- Educate patients and their families about diabetes foot care. Involving the entire family and caregivers in diabetes education may help improve adherence and reduce amputation rates.
- Show patients how to prevent diabetic foot ulcers. Foot ulcers increase the risk of amputation, especially when not treated. Teach patients, their caregivers, and their families about the steps they can take to prevent diabetic ulceration.
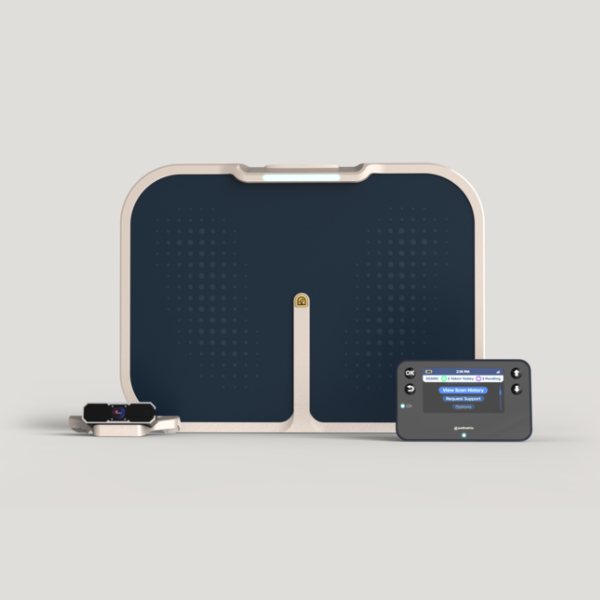
- Consider remote temperature monitoring (RTM). Easy-to-use RTM programs, such as the Podimetrics SmartMat™ Program, may help prevent diabetic foot ulcers in underserved populations at risk for amputation.
Delivering optimal diabetes care across cultures begins with understanding and respecting diverse values, perspectives, and communication needs. By embracing these principles, providers can build trust, enhance patient outcomes, and reduce the risk of complications like ulceration and amputation.
Visit our Providers page to learn more about how the Podimetrics SmartMat Program can help your patients manage their conditions conveniently at home and reduce their risk for amputation.