Why do vision loss and amputations, two very different complications of diabetes, often go hand in hand? This connection is especially timely to recognize during National Eye Exam Month, a reminder of how closely vision health ties into overall diabetes care.
At first glance, eyesight and foot health could not seem farther apart. Yet for millions of people living with diabetes, problems in the eyes and problems in the feet often share the same root cause. Both are tied to small blood vessel damage that builds up over time when blood sugar levels remain too high. That damage may first appear in the form of blurry vision or changes in the retina, but it can just as easily show up as numbness or wounds on the feet. In fact, research shows that people with diabetic retinopathy are 2 to 4 times more likely to also face diabetic foot ulcers (DFUs) or amputations.
When you pause to think about that, the connection becomes more striking. These two outcomes may seem unrelated, yet they tell us a very similar story about what is happening inside the body. The story is one of tiny vessels breaking down and nerves struggling to function, a story that unfolds quietly but powerfully.
A Shared Path: Retinopathy and Neuropathy
The relationship between diabetic retinopathy and diabetic peripheral neuropathy is not just coincidence. Both are driven by the same process of microvascular disease. Over time, uncontrolled blood sugar damages the lining of small blood vessels, starving tissues of the oxygen and nutrients they need. In the retina, this shows up as leaking or blocked vessels that lead to vision loss. In the feet, it means nerves that no longer feel pain or temperature properly, leaving wounds unnoticed until they become serious.
Research from PubMed has shown that retinopathy and neuropathy often develop in parallel. This connection can be eye-opening for patients who have never been told that what happens in one part of the body is a signal of what may happen in another. It reinforces the idea that diabetes care is not about treating isolated symptoms. It is about looking at the whole person.
How Vision Loss Raises the Risk of Foot Ulcers
The risks go even further. Beyond the shared biological pathways, vision loss itself can directly increase the likelihood of foot complications. Patients with low vision may not see the early signs of redness, swelling, or cuts on their feet. A small injury that would be obvious to someone with clear eyesight may be missed until it becomes infected.
For someone who is already dealing with vision loss, the challenges of self-care multiply. Imagine trying to check your feet every night when you cannot clearly see them. Now imagine also living with neuropathy that reduces your ability to feel pain. It is like losing both warning systems at once.
This creates a dangerous cycle. Poor vision reduces the ability to notice early problems, and neuropathy reduces the ability to feel them. By the time either issue is detected, it may already be advanced. That is why care teams emphasize not only treating vision or foot problems individually but also understanding the overlap between the two.
The Bigger Picture: Whole-Person Prevention
If this sounds discouraging, it should also be reassuring to know that prevention is absolutely possible. Diabetes care today is not just about managing blood sugar levels but about creating a system of checks and supports that catch small issues before they grow.
Regular dilated eye exams and routine foot assessments remain two of the most effective tools for preventing complications. These visits do more than confirm whether vision is stable or feet are intact. They act as early warning systems for the entire body. If one shows signs of trouble, it should immediately prompt a closer look at the other.
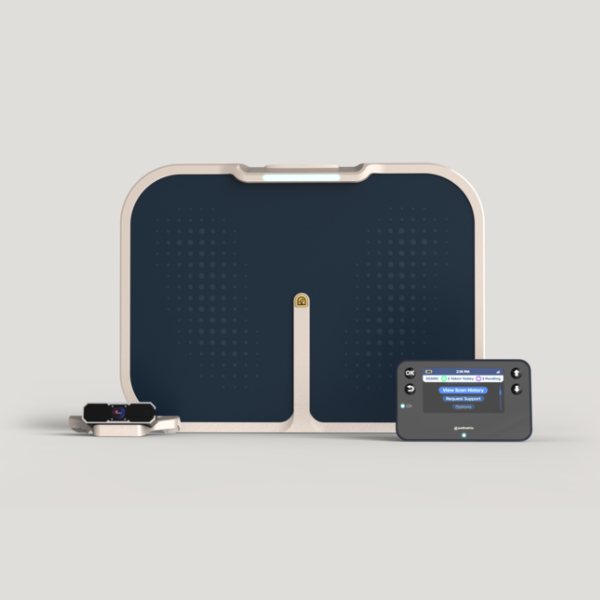
Technology is also playing an increasingly important role. For patients already living with vision loss, having daily temperature checks through remote foot monitoring ensures foot problems are identified early, even if they cannot see changes themselves. By tracking changes in temperature or inflammation, these tools can identify risk before it turns into a wound. That proactive approach not only protects the feet, it also reassures patients and families that they are not left to manage everything on their own.
When we think about prevention in this way, it becomes less about treating individual organs and more about treating the person. The eye and the foot may seem like distant neighbors in the body, but in diabetes they share the same fragile foundation. Supporting one means supporting the other.
For patients, understanding this connection can be life changing. A conversation at the eye doctor may lead to earlier foot screenings. A conversation at the podiatrist may lead to a referral for a dilated eye exam. Each touchpoint is an opportunity to prevent devastating outcomes like blindness or amputation.
Taking the Next Step
Eye care and foot care are not separate checkboxes on a list. They are part of the same story of diabetes and how it affects the body. By pairing regular vision exams with proactive foot monitoring, patients can stay ahead of complications that otherwise take too much away from quality of life.
Ready to take the next step? Discover how proactive foot monitoring supports whole-person diabetes care.