Falls are one of the most dangerous and overlooked complications of diabetes. Each year, one in three adults aged 65+ experiences a fall, and half will fall more than once. For people living with diabetes, the risk is even higher, and the outcomes are often more severe.
A single fall can mean a fracture, a hospital stay, or the beginning of a long decline in independence. The CDC estimates these injuries add up to more than 50 billion dollars in direct medical costs each year.
For too long, falls have been treated as accidents, the kind of thing that simply comes with age. In truth, falls are not random. They are the result of very real and very preventable health factors that podiatric care can help address.
Why Diabetes Raises Fall Risk
Balance is not a single function. It depends on nerves, muscles, joints, vision, and quick reflexes working together. Diabetes touches nearly all of these systems, leaving patients more vulnerable.
Neuropathy, which affects more than half of people with diabetes, quietly strips away sensation in the feet. Without that feedback, the body cannot react quickly when balance is challenged. Retinopathy, affecting up to 40 percent of patients, limits vision and makes navigation through daily life less safe. Muscle weakness and even cognitive changes, both more common in diabetes, compound the problem. Older adults taking multiple medications flagged as drugs that increase fall risk may face a 20-30% higher risk of falls. And for patients already coping with foot ulcers, the likelihood of falling is twice as high.
This combination of risks turns ordinary environments into hazards. A rug edge, a dim hallway, or a missed step can trigger a fall that changes a person’s life.
Podiatry’s Role in Prevention
Falls may begin with the feet, but so does prevention. Research has shown that podiatric care is a practical and effective way to reduce fall risk. In a randomized controlled trial published in the BMJ, older adults with disabling foot pain who received a podiatry-led intervention experienced 36 percent fewer falls over 12 months compared to usual care. The program combined orthotics to relieve pressure, guidance on safe footwear, a home exercise plan to strengthen the ankles and toes, routine podiatry visits, and education on reducing risk in daily life. Participants also improved their strength, ankle flexibility, and balance. These changes not only prevented injuries but also helped preserve independence.
Practical Steps for Patients
The most effective prevention strategies combine medical care with daily habits. Patients with diabetes can make meaningful changes that reduce their risk of falling.
- Wear supportive shoes with proper fit, and add orthotics or inserts when recommended.
- Build strength in the feet and ankles through simple stretching, resistance, and balance exercises.
- Review medications regularly with a provider, especially if they cause dizziness or fatigue.
- Get vision and hearing checked each year to catch subtle changes that affect stability.
- Make daily self-checks a routine, whether that means looking for changes in the feet, tracking small shifts in balance, or using simple tools at home that encourage consistency.
None of these steps require dramatic lifestyle changes. Taken together, however, they can transform the way patients move through the world.
Catching the Warnings Before the Fall
One of the most concerning realities of falls is how often they give warning signs. Unsteadiness while standing, hesitation when walking, or the habit of steadying oneself on furniture are all red flags. Too often, these early signals are missed or ignored until a serious fall occurs.
Annual screenings are important, but they are not enough on their own. Fall prevention works best when it becomes part of daily life, reinforced by providers, caregivers, and the patients themselves. Intervening early, before the first fall, can mean the difference between ongoing independence and a preventable crisis.
Building Stability from the Ground Up
Falls do not happen without cause. They are often connected to the same complications that put the feet at risk, such as neuropathy, ulcers, and loss of sensation. When patients pay attention to their feet each day, they also take an important step toward protecting their balance.
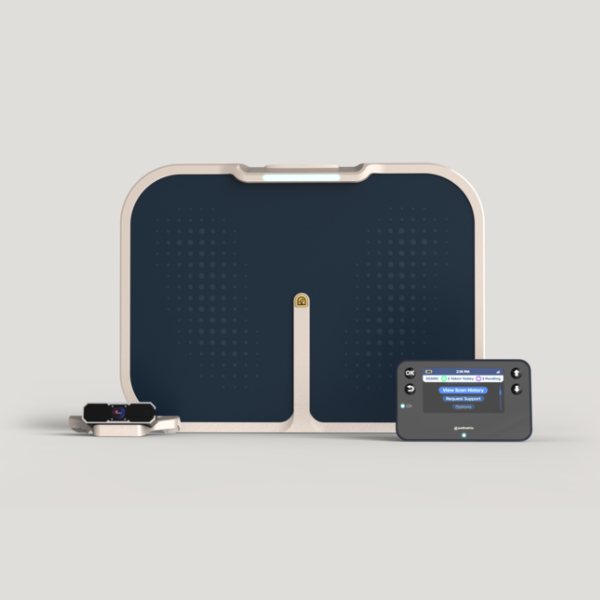
The Podimetrics SmartMat™ Program shows how this can work in practice. By helping identify early warning signs of inflammation, the program helps prevent wounds before they form. Just as importantly, it creates a daily habit of awareness. Each scan is a reminder that foot health is directly tied to mobility and stability.
When prevention begins at the ground level, we not only reduce the risk of diabetic foot complications but also address one of the root causes of falls.
Turning Awareness into Action
On this Falls Prevention Awareness Day, we are reminded that falls do not have to be a normal part of aging with diabetes. They are preventable, and prevention is possible.
Providers can ask the right questions, look for early signs, and integrate foot health into fall prevention strategies. Patients can make simple choices that protect their independence. Families and caregivers can encourage safe environments and reinforce daily habits that keep loved ones strong.
The path forward is clear. By treating falls as a serious complication of diabetes, and by acting early, we can reduce injuries, preserve mobility, and improve lives.
At Podimetrics, we partner with individuals and care teams to catch early signals before small problems become big ones. Visit podimetrics.com to find out how daily attention to foot health becomes a meaningful path toward safe, active living.