For people living with Type 2 Diabetes, the effects often ripple throughout the entire body putting vital organs like the heart under serious pressure.
As it turns out, over 30% of all people with Type 2 Diabetes eventually develop cardiovascular disease, and it is the leading cause of death in this population. The hidden danger is that heart conditions often don’t come with the “classic” signs like shortness of breath or chest pain. Many people don’t realize they have heart issues until a life-changing event, like a heart attack, stroke, or hospitalization, forces action. But by the time symptoms are severe enough to land a patient in the emergency room, the window for prevention has already closed.
The good news is that you don’t have to wait for a life-threatening event to know your heart is at risk. The body often gives early warning signs, but they don’t always show up where we expect. For people with diabetes, some of the most telling clues about heart health are found far from the chest: they begin in the feet.
Diabetic Foot Ulcers: A Visible Sign of a Hidden Problem
When we think about early signs of heart disease, feet are probably not the first thing that comes to mind. But foot wounds, particularly diabetic foot ulcers (DFUs), are far more than a localized issue.
A 2024 meta-analysis examining over 8,000 patients with DFUs found that nearly 45% had ischemic heart disease, 25% had congestive heart failure, and they were more than twice as likely to die from cardiovascular causes compared to diabetic patients without foot ulcers. These numbers tell a clear story: DFUs serve as an important warning sign of underlying cardiovascular problems.
But how exactly are DFUs and heart complications linked? The relationship is rooted in how diabetes affects the vascular system. A comprehensive review published in the Journal of Diabetes Research explains how diabetes damages the blood vessels throughout the body. This process impacts both large arteries supplying the heart (leading to heart attacks and heart failure) and the smaller blood vessels in the lower extremities (leading to DFUs). What appears as a small wound on the foot is often a visible reflection of the same vascular damage that puts patients at risk for heart attacks and strokes.
A 2022 study, co-authored by Jon Bloom and Dr. Gary Rothenberg of Podimetrics, found that rates of congestive heart failure increased from 38% to 65% during DFU episodes, and myocardial infarction rates nearly doubled. This isn’t a coincidence — it reflects how a DFU is often a red flag that cardiovascular disease is actively worsening, even if patients haven’t yet experienced classic symptoms like chest pain.
As Dr. Michele Esposito, a practicing heart failure cardiologist, explains:
“Diabetes and cardiovascular disease are highly comorbid. Complications from one can directly impact and even worsen the other. Unfortunately, practitioners for each condition – whether it be endocrinologists, vascular surgeons, or cardiologists—are typically siloed and rarely in direct communication with one another; this makes efficient diagnostic or therapeutic intervention more cumbersome. That’s what makes Podimetrics unique and invaluable to our patients. They create a bridge that allows patients to be managed more efficiently on both ends, with the ability to prevent downstream complications.”
When DFUs progress, they often lead to lower extremity amputations, and the cardiovascular burden only grows from there. Limb loss dramatically increases the energy required for basic movement. Below-knee amputees expend up to 33% more energy when walking, while above-knee amputees expend up to 65% more energy. For patients already living with heart disease, this added strain can accelerate heart failure and increase mortality risk. But it’s not just about the physical toll. Amputations also come with psychological and lifestyle impacts, including depression, social isolation, and reduced mobility which can indirectly worsen cardiovascular health. This cycle, where vascular damage leads to DFUs, amputations, and heart failure, is a dangerous spiral that often goes unrecognized until it’s too late. In this way, a DFU is not just a predictor of amputation, but a catalyst for a dangerous cycle where the cardiovascular system becomes increasingly overtaxed, until it’s too late.
The Case for Proactive, Multidisciplinary Care
Despite this clear connection, DFUs often aren’t treated with the urgency they deserve. Many patients with DFUs, and even their providers, fail to realize that a foot wound can be a harbinger of heart disease. A 2024 Harris Poll revealed that many people with diabetes don’t consider themselves at risk for heart complications at all.
Managing a diabetic foot ulcer requires a team effort across specialties. A DFU patient isn’t just a podiatry case; they require coordinated management that includes cardiology, endocrinology, nephrology, mental health, and wound care teams. A foot ulcer should trigger a system-wide cardiovascular investigation, not just localized wound treatment.
In a recent example from Dr. Gary Rothenberg, Podimetrics Director of Medical Affairs, a patient presented with what seemed like a minor heel crack. A routine vascular assessment revealed significantly reduced circulation, leading to further cardiac workup. The result? A quadruple bypass surgery that likely saved his life. As Rothenberg explained,
“Without that foot exam, his heart condition might have remained hidden until it was too late.”
Unfortunately, not every patient receives that crucial foot exam in time. Early warning signs of DFUs often go unnoticed until they escalate into serious complications. This is where proactive, team-based monitoring can make a real difference. By identifying these early signs, care teams have a chance to intervene before a wound develops, reducing the risk of hospitalizations, amputations, and worsening heart health.
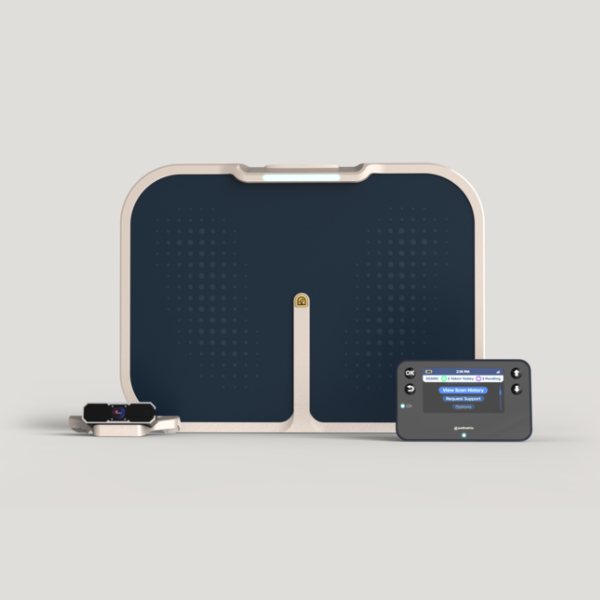
At-home monitoring programs, such as Podimetrics’ SmartMat™, support this proactive approach by giving clinicians early insight into changes that might otherwise remain hidden. Identifying problems sooner allows care teams to protect not just foot health, but overall cardiovascular wellbeing.
Prevention Starts from the Ground Up
The story of diabetic foot ulcers is often told in hindsight: after the wound, after the amputation, after the heart attack. But it doesn’t have to be that way.
Every DFU presents an opportunity to act early, to uncover the silent problems quietly building beneath the surface long before they spiral into a medical crisis. Prevention is not simply about reacting to emergencies, but rather about recognizing subtle signs and stepping in with timely intervention. It requires a proactive approach that prioritizes monitoring, education, and coordinated care across specialties.
If we shift the focus from treating complications to preventing them, we have the power to stop the cycle of DFUs, amputations, and heart failure before it begins.