Discover actionable strategies to reduce diabetes distress and improve care for patients and caregivers alike.
Living with diabetes means navigating a relentless daily routine of blood sugar monitoring, medication management, dietary restrictions, and constant vigilance against complications. For many, this burden becomes more than just medically challenging—it becomes emotionally overwhelming. Yet, healthcare systems continue to treat diabetes distress as a side note rather than a central component of comprehensive care.
The numbers tell a stark story: nearly one in three people with diabetes experiences diabetes distress, with up to 48% of patients facing this challenge within an 18-month period.¹ Despite affecting between 18% and 40% of patients at any given time, diabetes distress remains significantly underrecognized and inadequately addressed across our healthcare ecosystem.
Studies show that individuals living with type 1 or type 2 diabetes are at increased risk for depression, anxiety, and eating disorder diagnoses. There are nearly 30 million people in the United States diagnosed with diabetes, and more than 57 million people living with a mental health disorder. While people with diabetes are up to three times more likely to have depression than other populations, only about half ever receive treatment for their mental health concerns.
What is Diabetes Distress and Why It’s Different from Burnout
Diabetes distress isn’t simply feeling tired of managing a chronic condition. It’s a complex psychological state where the emotional, logistical, and interpersonal demands of diabetes management become so overwhelming that patients experience reduced self-care efficacy. Unlike clinical depression, diabetes distress is often an inherent part of living with diabetes due to the disease’s relentless daily demands.
“Diabetes distress isn’t just burnout. It’s chronic stress tied to living with a demanding condition that can feel overwhelming emotionally, socially, or logistically,” explains Dr. Jairo Arce Morales, Assistant Professor of Psychiatry and Behavioral Health at Montefiore Einstein. “Addressing it improves both mental and physical health. The mind and body are truly interconnected.”
Overall, diabetes distress may affect up to two-thirds of people with diabetes, with severe distress in approximately one in five. A recent Podimetrics survey of Medicaid beneficiaries with diabetes revealed that 65% are also living with behavioral health conditions, including depression, anxiety, and loneliness. Four in 10 feel that these conditions exacerbate challenges with diabetes management.
The triggers are as varied as they are persistent:
- Daily management challenges: Multiple medications, frequent glucose monitoring, and physical discomfort from injections
- Emotional impact: Mood swings, chronic stress, and limited emotional support systems
- Healthcare navigation barriers: High costs, insurance complications, appointment delays, and equipment access issues
- Complication fears: Anxiety about diabetic foot ulcers, vision loss, and kidney disease
- Life disruption: Financial pressure, workplace challenges, and family relationship strain
Why System Problems, Not Patient Problems, Drive Diabetes Distress
Here’s where the traditional healthcare approach falls short: When providers encounter patients who seem disengaged or “non-compliant,” the standard response is often a behavioral health referral. While mental health support is crucial, this approach treats diabetes distress as purely a psychological issue rather than recognizing it as a systemic problem rooted in our fragmented, overly complex healthcare system.
The reality is that even excellent mental health professionals cannot fully address diabetes distress alone. The condition stems from real, tangible challenges within how we deliver diabetes care—challenges that every member of the care team must recognize and work to eliminate.
Consider the experience of a 46-year-old social worker who, despite her mental health background, began withdrawing from care after several toe amputations. Her resistance to traditional therapy wasn’t about denial—it was about feeling overwhelmed by a system that seemed to create more obstacles than solutions. It was only through the trusted relationship with her podiatrist, who met her where she was and worked to simplify rather than complicate her care journey, that she eventually re-engaged with her full care team.
How Care Teams Can Address Distress Beyond Referrals
Every healthcare professional interacting with patients with diabetes has a role in addressing their distress. This doesn’t mean every provider needs to become a therapist, but it does mean recognizing that small changes in approach can have a significant impact.
Reframe the conversation: Instead of asking, “Is it hard to wear your diabetic boot every day?” (the answer is obviously yes), try “What’s the hardest part about wearing the boot, and how can we make it less difficult?” This simple shift invites problem-solving rather than just complaint.
Leverage underutilized resources: Certified Diabetes Care and Education Specialists (CDCESs) serve as crucial bridges between clinical care and emotional support. These “diabetes coaches” are specially trained to help patients build confidence in self-management while navigating the emotional aspects of diabetes. Yet they remain underutilized in many healthcare systems.
Address screening gaps: Despite American Diabetes Association recommendations, validated tools like the Diabetes Distress Scale (DDS) and Problem Areas in Diabetes (PAID) are rarely used in routine care. Many providers rely solely on general depression screening tools like the PHQ-9, which can miss diabetes-specific distress entirely.
Using Technology to Simplify, Instead of Complicate Routines
When designed thoughtfully, technology can significantly reduce diabetes distress by lightening the cognitive and emotional load of daily management. Remote patient monitoring solutions, continuous glucose monitors, and caregiver-connected tools can provide structure, timely insights, and peace of mind.
However, technology implementation must follow three critical principles:
- Choose simplicity over complexity: Technology should solve problems, not create new ones
- Foster connection: Patients engage more when they feel seen and supported through their tech tools
- Honor the human experience: Offer flexibility and breathing room—even the best tools aren’t helpful if they create additional stress
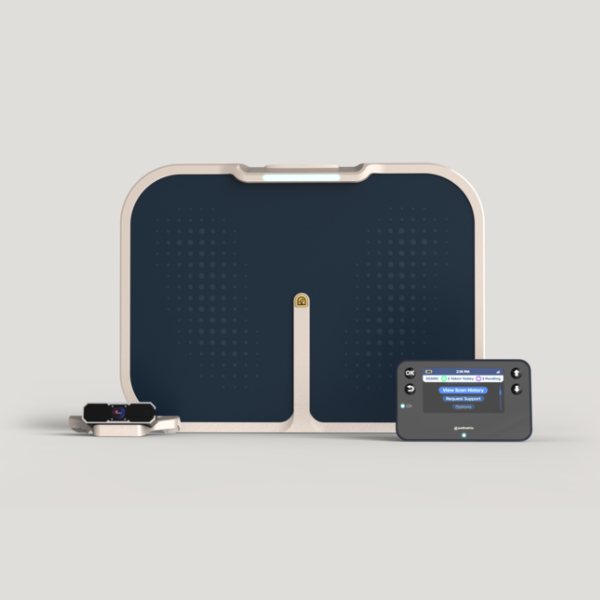
Programs like remote foot monitoring can help patients and care teams proactively intervene before small issues escalate into major complications. This kind of support is especially impactful for patients managing complex conditions or facing mobility barriers.
Why Addressing Diabetes Distress Makes Financial Sense
The financial implications of unaddressed diabetes distress are substantial and far-reaching:
For Healthcare Systems and Payors: People with both diabetes and behavioral health conditions cost the healthcare system nearly $3,000 more per year than those with diabetes alone. Diabetes distress drives poorer medication adherence, worse glycemic control, and higher complication rates—all translating to significantly higher costs.
For Employers: Employees living with diabetes are twice as likely to experience depression, anxiety, and stress, contributing to reduced productivity and increased absenteeism. The annual cost of lost productivity due to diagnosed diabetes in the U.S. is estimated at $90 billion, with diabetes distress exacerbating this impact.
For Providers: When patients appear disengaged, providers often experience their own version of frustration and burnout. Many primary care providers report feeling confident in their ability to manage the psychological aspects of diabetes care, creating a confidence gap that limits timely intervention.
Why Caregiver Support Directly Impacts Patient Outcomes
US-based research demonstrates that caregiver strain and burnout are closely linked to poorer patient outcomes in diabetes care. For example, studies show that when caregivers experience high levels of stress, patients have worse diabetes management behaviors and metabolic control. Conversely, caregiver involvement in education and support programs leads to improved patient HbA1c, better adherence to self-care, and enhanced psychological well-being.
What Healthcare Organizations Need to Do Next
Addressing diabetes distress isn’t just a clinical necessity—it’s a shared responsibility across the entire healthcare ecosystem. The solution requires:
Provider Training and Tools: Empowering clinicians with validated assessment tools and team-based workflows for behavioral integration
System Simplification: Reducing complexity in every patient interaction rather than adding layers of referrals and requirements
Technology Integration: Implementing patient-centered, tech-enabled solutions that foster connection and reduce burden
Whole-Team Approach: Recognizing that every care team member, from specialists to care coordinators, plays a role in recognizing and reducing distress
Value-Based Strategies: For payors, covering integrated behavioral and medical care models that reimburse for proactive interventions
Moving from Recognition to Action
The prevalence of diabetes distress—affecting up to two-thirds of people with diabetes—demands that we move beyond treating it as an afterthought. Organizations that simplify care through data-driven insights, seamless team collaboration, and patient-centered tools will lead the way in transforming diabetes care from a source of distress into a model of connected, compassionate healthcare.
By acknowledging that diabetes distress is often rooted in systemic inefficiencies rather than individual failings, we can work collectively to make meaningful changes. Small shifts in how we communicate, coordinate care, and leverage technology can have profound impacts on patient outcomes, provider satisfaction, and healthcare costs.
The goal isn’t to eliminate the inherent challenges of living with diabetes—that’s unrealistic. The goal is to ensure that our healthcare system supports rather than compounds those challenges, creating an environment where patients feel empowered rather than overwhelmed in their diabetes journey.
Want to take a deeper dive?
Download our full white paper to explore real-world strategies for identifying and addressing diabetes distress across the care continuum.
About the Author
The Podimetrics Editorial Team collaborates with clinicians, product experts, and healthcare writers to bring timely, accurate, and practical insights to those working in and affected by complex diabetes care. Our goal is to simplify key challenges in diabetic foot health and support whole-person outcomes. Thank you to the authors of the white paper, Dr. Gary Rothenberg and Dr. Denise Levy, for their clinical expertise and valuable insights on this significant topic.