By: Mike Doane, Arcadia
This guest post is contributed by Arcadia, a leading data platform for healthcare organizations, helping providers harness data for better patient outcomes.
For patients living with chronic diseases, necessary care extends beyond the walls of a provider’s physical office. Diabetes management, for example, requires ongoing vigilance to prevent serious complications (like amputation) and the financial and emotional tolls that come along with them. Providers need real-time insights into their patients’ daily lives to change this trajectory.
Research suggests that patient-generated health data (PGHD) — data created, captured, and recorded by patients between appointments — has the potential to improve health outcomes. Providers can identify risk factors early and intervene proactively by leveraging remote device-generated clinical data, health history, social determinants of health (SDoH), and other patient-reported information.
This article explores how providers can harness PGHD to improve health outcomes and reduce complications.
Benefits of Leveraging PGHD
According to the Assistant Secretary for Technology Policy (ASTP) for Health Information Technology, patient-generated health data (PGHD) can supplement existing clinical data, providing a comprehensive picture of ongoing patient health by surfacing:
- Health history
- Treatment history
- Biometric data
- Symptoms
- Lifestyle choices
When patients capture and share this data, providers can better gauge patient health between medical visits and make informed decisions about preventive and chronic care management. Remote monitoring also makes care more accessible by allowing providers to spot issues early on without requiring the patient to travel to and from their clinic.
PGHD supports improved care quality, coordination, and cost. However, achieving these outcomes requires patient engagement and proper data management, meaning providers must strategically implement PGHD strategies.
How to implement PGHD for improved outcomes
1. Develop a workflow
First, providers must develop internal workflows for collecting, analyzing, and acting upon PGHD. A comprehensive plan will consider the following:
- What methods and technologies will patients use to collect PGHD?
- How will patients securely share PGHD with your team?
- Who has permission to access PGHD once patients share it?
- What processes will your team use to validate PGHD?
- How will your organization use PGHD insights? (i.e., for research, care delivery, etc.)
A well-planned approach to implementing PGHD prepares all parties involved to collect and utilize data for the sake of the patient’s health. Provide ongoing support for care teams and research staff, including explaining how to use any necessary software and integrate it with your existing systems. In addition to providers and patients, caregivers must also receive guidance for using PGHD technologies and understanding their results.
2. Encourage patient participation
Next, identify which populations will be the main focus of PGHD implementation. Providers may recruit patients for PGHD collection using the following methods:
- In-person consultation: Recommend PGHD to eligible patients during office visits, using this time to explain the process’s usefulness in patients’ care journeys and answer any questions
- Marketing emails or patient portal messages: Reach a broader audience by introducing PGHD technologies in mass messages, emphasizing the value of tracking this data as a tool to protect patient health
After enrolling interested patients, set clear expectations about how to use PGHD technologies, how a patient’s care team will respond, and how you’ll protect patient data privacy.
3. Adopt relevant technology solutions
In addition to remote monitoring devices, providers should adopt helpful data analytics tools to transform patient-collected data into actionable insights. The right technologies should help providers store, organize, and analyze vast amounts of data to aggregate and act on all information — including real-world, clinical, and patient-generated data.
For example, care management software can unify SDoH data with other clinical data and PGHD to help care teams identify populations most in need of intervention. Since various SDoH factors (such as housing stability and transportation) can significantly impact a patient’s health outcomes, a provider’s view of the patient’s health would be incomplete with just PGHD. Implementing care management software enables providers to pinpoint at-risk populations and develop timely, appropriate interventions by analyzing a larger pool of data.
4. Review data and plan interventions
After collecting and integrating PGHD with other health data, providers can analyze this information to extract relevant insights and develop interventions accordingly. This step involves deploying proactive interventions to help mitigate adverse health events using data about a patient’s experiences, both in the office and at home.
For example, when PGHD suggests poor glucose control, a provider may contact their patient to warn them and inquire about medication adherence, stress levels, and other factors that could impact glucose levels. Then, the provider could connect the patient with relevant resources to get them back on track, such as financial assistance from a prescription discount program.
The key to efficient analysis is implementing tools that simplify data interpretation, including:
- Generative artificial intelligence (AI): Among recent health trends, solutions powered by generative AI stand out as a promising solution for improving patient engagement and adherence to treatment plans
- Data dashboards: Visualizing raw data points and long-term trends through customizable dashboards enables providers to monitor patients’ ongoing health statuses and forecast future trends
- Predictive analytics: According to Arcadia’s predictive analytics guide, this technology powers early reminders and helps providers encourage preventive care, such as screenings or vaccinations
Offering proactive approaches that equip patients and providers to work together toward preventive care ultimately results in improved health outcomes. Additionally, when providers proactively meet care needs, they can mitigate unnecessary costs.
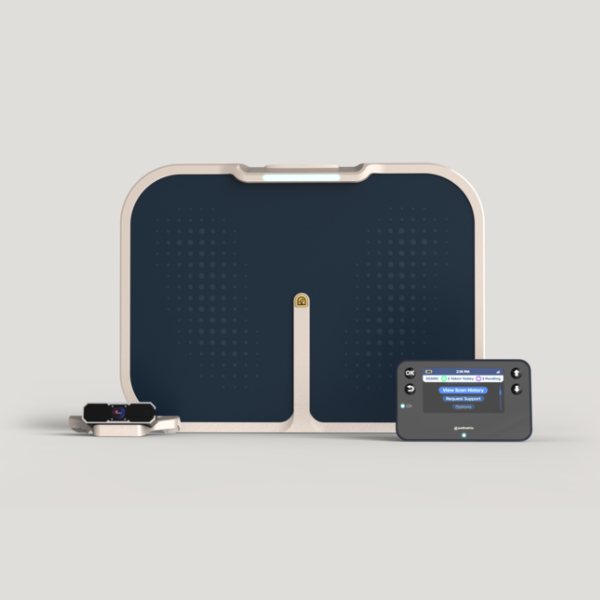
At Podimetrics, we leverage patient-generated health data by monitoring foot temperature through our in-home SmartMat. This data helps identify early signs of diabetic foot complications, enabling timely interventions and improved patient outcomes. By integrating PGHD with proactive care strategies, providers can better support patients managing chronic conditions like diabetes.
To learn more about how Podimetrics helps those living with complex diabetes, visit our homepage to explore the Podimetrics SmartMat™ Program.