What is thermometry?
Thermometry is the measurement of temperature, and it’s been used successfully for the prevention of diabetic foot ulcers since the 1970s. Its success has also been measured and evaluated in peer-reviewed studies.
Thermometry’s subsequent temperature guided avoidance therapy is now recommended in clinical practice guidelines for high-risk patients with diabetes from the following authorities: The International Workgroup on the Diabetic Foot, The Wound Healing Society, and The American College of Foot and Ankle Surgeons.
When was it first used for diabetic foot complications?
In 1975, Dr. Paul Brand and his colleagues first recognized that inflammation of the foot was a precursor to foot complications in high-risk patients with diabetes mellitus. Inflammation would lead to ulceration or infection. Ulceration and infection would often lead to amputation.
Dr. Brand’s original research was focused on leprosy patients; however, the findings would impact diabetic foot care for years to come. By associating inflammation as a precursor to additional foot complications, temperature rises could be extracted as a signal of inflammation. When the foot is inflamed, the temperature in that spot will be higher.
Because temperature could so accurately predict and point out areas of inflammation, the practice of thermometry was initiated to detect hot spots with the hopes of staving off further complications like ulceration and infection (which could ultimately lead to life-changing amputation).
The original thermometry instrument was a self-held thermometer. Patients would need to apply the thermometer to several areas of their feet everyday to get readings themselves.
How effective is thermometry at detecting inflammation?
Outside of the initial study during the 1970s, more recent ones have confirmed thermometry’s effectiveness at the detection and prevention of diabetic foot complications.
In 2017, The Agency for Healthcare Research and Quality (AHRQ) found that home monitoring of foot skin temperature was proven to be effective for preventing incidence and/or recurrence of foot ulcers.
Thermometry has been studied in three randomized clinical trials (RCTs) with positive results: one in 2004, another by the same group in 2007, and additionally by another cohort in 2007. All three of these trials are considered evidence of thermometry’s effectiveness.
To drill down even further into metrics that prove success, the three RCTs reported a 70% mean relative diabetic foot ulcer reduction which was reflected in the clinical practice guidelines.
What solutions are available that use thermometry to prevent diabetic foot complications?
As technology continues to advance, thermometry applications for diabetic foot complications have become significantly more easy-to-use for patients.
There are several different ways that thermometry has been applied as a solution for the detection and prevention of diabetic foot complications. While self-held thermometers can still be used, innovative options have made thermometry much more effective and simple.
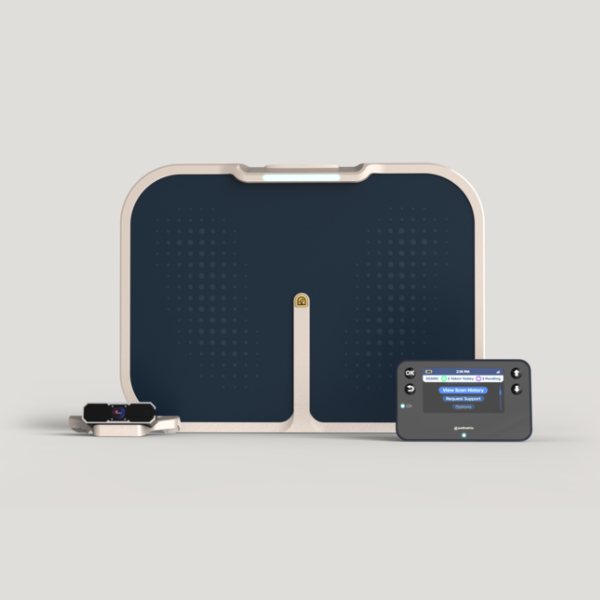
Modern thermometry solutions for diabetic foot complications include socks, insoles, and mats.
All of these options utilize sensors to measure temperature in the feet, sending the findings remotely to a system that can capture this data for analysis and, when necessary, intervention.
However, there are distinguishing features due to each form factor. With socks, patients are sent a fixed quantity and require consistent wear. The socks also need washing and care. Insoles can be customized for each patient, but mean that patients must be cognizant of securing the insoles in whatever pair of shoes they wear.
The use of a mat, however, has been proven to show higher than average engagement rates. Requiring only 20 seconds a day and resembling a bathroom scale, patients are comfortable using it. It’s a solution that can easily be integrated into a patient’s daily routine with lower levels of disruption or confusion.
A proven method for the prevention of diabetic foot ulcers.
Clinical research clearly demonstrates that thermometry is an effective, evidence-based method of preventing diabetic foot ulcers by monitoring the feet for changes in temperature that indicate inflammation. By watching for these temperature changes, diabetic foot ulcers can be caught much earlier (with the mat solution, up to five weeks before they would clinically present).
Thermometry should be a part of any prevention plan for diabetic foot complications, as it is quite successful at detection and can be woven into a patient’s care. For high-risk patients with diabetes, this early detection can be significant especially if it prevents further complications like life-altering amputations.