Heart failure (HF) remains a leading public health burden in the United States, with over 6 million adults in the US currently living with this chronic disease. Behind that number are everyday moments that signal a shift in health long before someone feels sick enough to seek care. It’s an older adult quietly adjusting swollen socks in the evening, a caregiver noticing wedding rings are harder to slip off, or a loved one seeing the numbers on the scale rise steadily. These simple moments often go unnoticed because they feel unimportant in the long list of tasks that come with managing a chronic illness. Yet they can be some of the earliest clues that HF is getting worse.
When Fluid Retention Becomes the First Red Flag
Despite medical advancements, the number of HF hospitalizations has been increasing over the last two decades, with recent reports indicating that over 1 million hospitalizations list HF as the leading diagnosis. Fluid retention, or edema, is one of the strongest indicators that the body is under stress, often preceding a more severe decline. Of all HF hospitalizations, it has been shown that approximately 90% are due to excess fluid in the lungs. Treatment relies on medications that help remove this fluid, but around half of patients remain at least partially congested sixty days after discharge. This pattern shows that the earliest stages of fluid buildup are being missed, and patients need better ways to monitor these changes before they turn into emergencies.
A Growing Burden on Families and the Healthcare System
HF places a significant economic and emotional toll on both the healthcare system and the families who navigate it, with projections of a 100% increase in total medical costs from 2013 to 2030. A national analysis from the Agency for Healthcare Research and Quality found that the average 30-day adult readmission costs about $15,200. For health systems, this rise translates to growing strain on hospital capacity and increased demand for chronic care resources.
For patients and families, each hospitalization brings missed work, transportation challenges, and the emotional weight of living in constant uncertainty. Caregivers often take on new responsibilities overnight, impacting their own health, income, and stability. Patients may lose independence, feel anxious about returning home, or fear that the next episode will be worse than the last.
It Doesn’t Appear Suddenly: The Early Clues Matter
A study published in Circulation by Chaudhry and colleagues showed how early fluid-related weight changes begin in HF. By tracking patients’ daily weights, the researchers found that those who were later hospitalized started gaining weight weeks before they became acutely ill. The trend became most noticeable in the final week before admission, when small increases of just a few pounds were strongly linked to hospitalization. The study made it clear that fluid retention does not appear out of nowhere. It develops gradually and offers a measurable early warning that care teams can act on.
Being alert to even small physical changes can be the difference between a peaceful evening at home and an urgent hospital visit. But the patients who stand to benefit most from early monitoring are often managing multiple complex conditions, which means subtle shifts in weight or swelling can easily get lost among everything else they’re juggling. Trying to keep track of medications, appointments, and the day-to-day realities of living with chronic illness makes it much harder to notice a few extra pounds or slightly tighter shoes and even harder to understand what those small changes might be indicating.
What the Research Shows About Early Monitoring
This is exactly when early monitoring can help, turning those easily missed clues into something care teams can act on. Evidence also shows that remote monitoring programs that combine daily weight tracking with structured nurse outreach can meaningfully reduce readmissions and improve quality of life. These programs work because they shift the responsibility from patients noticing subtle symptoms on their own to a more reliable system that monitors early changes and follows up promptly.
This is supported by a systematic review published in Patient Education and Counseling by Helena and colleagues. The authors evaluated nurse-led HF education and disease-management programs by reviewing randomized controlled trials where adults with HF received structured, one-to-one education or follow-up from a nurse while living independently in the community. The findings showed that patients who received nurse-led support experienced fewer readmissions, fewer hospitalizations, lower healthcare costs, and better overall quality of life.
Additional evidence comes from a randomized clinical trial published in BMJ Innovations by Aniket Zinzuwadia and colleagues. The study followed 190 adults recently discharged with cardiovascular disease who were enrolled in a structured virtual cardiology program. This program blended routine chart review by a dedicated care team, symptom assessment, remote monitoring of vital signs, including daily weight, medication titration, and ongoing patient education. Compared to patients who received standard outpatient cardiology care, those in the virtual program experienced significantly lower cardiac and all-cause readmission rates over the ninety-day follow-up period.
This combination of automated weight monitoring and nurse-led triage reflects the evidence behind successful remote monitoring programs. The system does not depend on patients to notice subtle day-to-day changes or decide when something feels wrong. Instead, technology captures the early signal, the clinical team confirms relevant associated clinical findings, and care is escalated only when symptoms suggest that intervention may be needed.
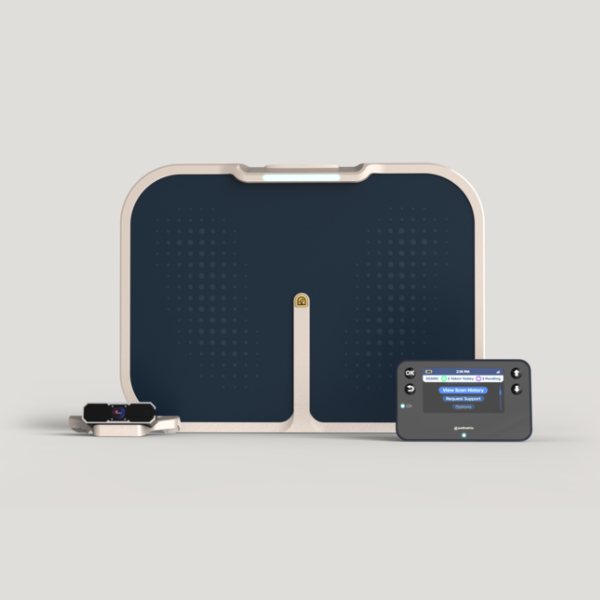
The Podimetrics SmartMat+ Program takes these principles and applies them in a way that is practical for everyday life. The SmartMat+ captures a patient’s weight during a simple daily foot scan and sends the reading to the Podimetrics clinical team. When the system detects a meaningful increase in weight, a nurse reviews the trend, checks in with the patient, and assesses symptoms such as swelling, shortness of breath, or fatigue. Based on that conversation and the clinical protocol, the nurse determines whether the patient needs closer follow-up or a visit with their provider. For people managing several chronic conditions at once, this kind of quiet, consistent support can make it easier to recognize early signs of worsening HF. It gives care teams clearer insight into day-to-day changes and offers patients a way to stay connected to their care before small shifts become more serious events.
Choosing Care Over Crisis
The evidence shows that consistent weight monitoring and thoughtful clinical follow-up can help patients stay stable at home and avoid the stress and disruption that come with repeated hospitalizations. These approaches give families clearer guidance, help care teams act sooner, and offer patients a sense of steadiness in a condition that can feel unpredictable.
Paying attention to fluid retention is ultimately about creating room for earlier care and greater peace of mind. When we recognize these subtle signals and respond with support rather than urgency, we give people living with HF a better chance to remain comfortable, independent, and connected to the lives they want to lead.