In the height of the COVID-19 pandemic’s first year, 2020, telehealth started booming. Big time. While platforms like Teladoc and MDLIVE have existed since before the pandemic, they certainly saw an uptick in usage while the majority of the nation’s population huddled indoors. In fact, some of their stock soared, reflecting murmurs in the industry that telehealth for diabetes and virtual medicine was the future.
But according to Fast Company in early 2022, telehealth startup stocks had fallen — and people are trying to figure out what comes next. “At the height of the pandemic, the value proposition of remote care was obvious. But now, everyone is trying to figure out where telehealth fits into the overall healthcare landscape,” writes Ruth Reader.
And it’s a great question.
Did telehealth die off?
At the start of 2022, telehealth seemed most popular for services like behavioral health, but there was a big question mark around it for other areas, like primary care. Early investment trends showed that people did want to see their doctors in person — but they wanted it to be easier. What did that mean? It wasn’t quite clear.
Now we’re seeing more studies around telehealth coming out of the last two years of data. And it is pretty clear that virtual care is here to stay.
A quick Google search will reveal many articles that demonstrate the effectiveness of telehealth in several areas of medicine. As mentioned before, telehealth for behavioral health and mental health is going to continue. But there’s even been early research on the success of telehealth for high-risk pregnancy.
But we’re seeing telehealth applied to some of the core issues facing our nation’s health care system. For example, telehealth allowed Black patients to access as many visits as non-Black patients. This equalizing potential gives telehealth promise. Additionally, there’s promise for rural patients. Can it help bridge the gap within health inequity? If at all possible, telehealth for diabetes seems clearly worth a try.
What makes telehealth successful?
Telehealth, telemedicine, virtual care, and digital medicine (all interchangeable terms, by the way) are dependent on several factors to be successful.
1. Delivery method
How is it delivered? Some require apps. Others use desktop platforms. In many cases, these delivery methods do rest on the availability of reliable broadband access. This isn’t something everyone has. In fact, many of those same populations who suffer from health disparities also can’t access or afford Wi-Fi.
2. Interoperability
For telehealth to work well, it needs to speak with other systems commonly used in health care environments. Depending on the model, it might require APIs to push data back and forth into EHRs and other databases or platforms.
3. Funding
One of the biggest hurdles for a successful telehealth program is funding. That’s why we’re seeing more bills move through Congress to support telemedicine. It’s also why many states are taking it into their own hands after seeing widespread success during the early years of the pandemic.
How can telehealth be better designed to meet the needs of its patients? Hint: It’s hybrid.
Much like hybrid work arrangements, what we’re seeing is a transformation in health care services that struggles to balance itself between technology-first digital platforms and the traditional, can’t-be-beat in-person experience.
In fact, it might be likely that companies will start to merge these components together to create a better customer experience: one that will cause an uptick in customer retention rates. After all, wasn’t it common ground to complain about long waits in doctor’s offices or hard-to-secure appointments?
With telehealth, appointments can (and have) become easier to make. Pharmacies can be linked to EHR systems. Notifications can be sent via text or app push. These changes can improve the overall experience.
But instead of thinking only telehealth or only in-person, hybrid concepts are most likely here to stay with success. Certain medical procedures and analysis simply can’t be done virtually, and there will be a need for in-person services.
At the same time, patients are now customers. And customers crave seamless, multi-channel experiences that anticipate their needs.
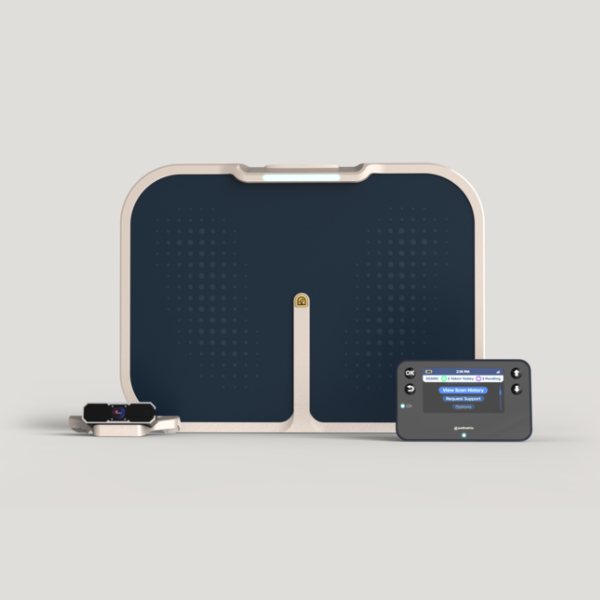
What works well digitally can stay digital. For example, remote monitoring devices have allowed patients to trim down their maintenance visits while still being under a watchful eye.
If these devices loop in a physical, in-person component, it’s only when necessary. This reduces the burden on patients who might have trouble getting to appointments, including those that live in rural areas or struggle with lack of transportation.
For these patients, it could make a huge difference. We’ve seen many medical devices successfully track patient risk from afar, and it’s only going to continue. This is a huge lift on the burden of preventive care, which we know is going to snowball due to the pandemic. With so many patients unable to make appointments or pushing them back because of safety, preventive care might have been skipped during 2020-2021.
While more patients are returning to in-person office visits, we still have a large dent to make up. And where preventive care services can be remote-first, it can also help providers deal with backlogs.
There’s a lot of promise with telehealth, especially telehealth for diabetes. As we move into more comfort and ease with leveraging these programs, adoption is likely to increase. And with the support of legislature, funding, and smart design, what can be done well in a virtual setting will probably stay virtual.