Diabetic amputations can be a heart-wrenching complication of diabetes. Their devastating effects extend not only to patients, but also to their families.
There’s a significant imbalance in the occurrence of diabetic amputations, with some groups experiencing much higher rates than others. For example, Blacks experience diabetic amputations at four times the rate of White Americans.
Between 2011 and 2016, minorities had the highest incidence of diabetes among racial groups, as discovered in a study. It analyzed population-based survey data from the U.S. National Health and Nutrition Examination Survey. The findings indicate that Blacks (20.4%), Latinos (22.1%), and Asians (19.1%) have the highest prevalence of diabetes among all races/ethnicities.
Social determinants of health (SDoH)—such as limited healthcare access, food insecurity, poverty, and discrimination—often perpetuate health disparities. Nonetheless, clinicians, and payors, can take steps to mitigate the risk of diabetic amputations by ensuring adequate preventive care.
What Are Social Determinants of Health ?
We often attribute health to lifestyle choices and genetics. But where you live, and your background can also play a critical role. This is known as social determinants of health, or SDoH, which are non-medical factors that can impact a person’s health. That includes their social and economic conditions, physical environment, education, and access to healthcare.
Health inequities, or disparities in health outcomes between different groups of people, can often be traced back to SDoH. These circumstances shape the health of individuals and the communities they live in. For instance, living in poverty can deprive people of nutritious food, access to care and health literacy. This, in turn, can lead to chronic illnesses like diabetes.
A review published in Pediatric Clinics of North America in 2020 found that children experiencing food insecurity display poor eating behavior. This behavior has the potential to lead to chronic diseases. By understanding and addressing these factors, healthcare providers can help improve health outcomes and reduce these inequities when caring for patients.
Tackling complex societal issues may seem daunting. However, with an optimistic and pragmatic approach, there can be great strides towards creating health equity.
The Link Between Health Inequity and Diabetic Amputations
The first step in addressing health inequity and diabetic amputations is to recognize the problem and its causes. The U.S. healthcare system has made significant strides in establishing effective diabetes management. With over 30 million people nationwide living with diabetes, it has become increasingly prevalent. Despite this, better healthcare has led to an improved prognosis for those who have access to it.
Yet, over 154,000 amputations occur every year in America—a 75% increase in the last decade. This highlights the brutal consequences faced by vulnerable populations and that health inequity persists.
The root of the problem? SDoH continues to play a significant role in determining health outcomes especially for minorities. They often face a disproportionate burden of chronic health conditions.
This is due to a complex array of factors, such as poverty and limited access to healthy foods. Educational gaps also play a significant role, as does lack of physical activity and limited access to quality healthcare.
Chain supermarkets and healthy food options are still significantly inaccessible to minorities, even in non-low income areas, for instance. Black neighborhoods have only 41% of the chain supermarkets found in White neighborhoods.
Native American communities face a difficult challenge. They have some of the highest poverty rates in the nation yet also struggle with food insecurity. At least 60 reservations in the U.S. are facing the challenge of food insecurity. Food insecurity may contribute to poor diet and mismanaged diabetes, resulting in uncontrolled blood sugar levels, diabetic foot ulcers, and amputation.
Amputation has been described as a “mega-disparity” that outstrips almost all other health disparities across races and ethnicities. Research has consistently revealed that Black, Latino, and Indigenous populations are at greater risk of diabetic amputation compared to their white counterparts. Latino Americans are at 1.5 times higher risk of amputation compared to Whites, whereas Indigenous Americans face twice the risk.
A study, published in 2022, highlights the disheartening outcomes faced by Black patients hospitalized with diabetic foot ulcers: almost 18% underwent major leg amputation or died within a month of being discharged. This percentage jumped to 18.3% for rural dwellers and 21.9% for those who identified as Black.
However, research has also revealed that targeted interventions aimed at addressing SDoH can help mitigate these disparities. The healthcare community needs to recognize the effect of the environment on the health of vulnerable populations. Then, take a multilevel approach to address them.
By considering social status, environmental factors, lifestyle, and biomedical information, health professionals can work towards lessening the health gaps associated with conditions such as diabetes. To achieve this, multidisciplinary teams must collaborate to influence community development and public services.
Accessible and Quality Diabetes Care
Improving access to quality diabetes care is a crucial step towards addressing health inequity and minimizing diabetic amputations.
Given diabetes is more prevalent in specific demographics—particularly people of color and those living in poverty—it’s vital to examine and address the underlying SDoHs that affect these groups.
It’s important for the medical community to collaborate and ensure patients are receiving the care they need to manage diabetes effectively and prevent complications. Tragically, every 3 minutes and 30 seconds in the U.S., a diabetic amputation occurs—and a staggering 85% of these cases are entirely preventable.
What kind of support can help these communities? This may involve providing additional resources, such as transportation to medical appointments, social workers to connect patients to community resources, or patient navigators to help guide individuals through the healthcare system.
In addition,payors can support these efforts by providing reimbursements for these types of services and incentivizing providers to provide high-quality care to all patients, regardless of their income or background.
Empowering Patients With Education
Patient education and engagement are also essential for preventing diabetic amputations. Patients with diabetes need to know how to manage their blood sugar levels, how to monitor for signs of complications, and when to seek medical care if something doesn’t feel right.
It’s crucial that patients are empowered to actively participate in their care, and that they feel comfortable asking questions and advocating for themselves when needed. Importantly, healthcare providers must demonstrate compassion and engage in thoughtful questioning during routine care visits. True, effective preventive care must consider how to talk to patients about these critical influences on their health. Taking the time to comprehend a patient’s lifestyle and community can enhance patient care by fostering a culture of health equity and removing the social barriers that impede well-being.
To prioritize SDoH in patient care, a comprehensive approach is key. Identifying and addressing these factors that impact patient health requires a multidisciplinary team, one that includes social workers, care coordinators, community partners, and healthcare professionals, working together to craft individualized care plans that address the full range of patients’ medical and nonmedical needs. With the correct approach, patients feel supported and empowered, confident to share challenges and take an active role in their healthcare.
Implementing the Changes Needed to Improve Health Equity
Finally, an important aspect of addressing diabetic amputations and health inequity is promoting broader societal changes to reduce inequity in healthcare access and outcomes.
This means advocating for policies that address the underlying SDoH, such as poverty, food insecurity, and lack of affordable housing. It also means working to eliminate discrimination and bias in healthcare settings, and promoting cultural competency and sensitivity.
For example, researchers have suggested an approach recently used to address health disparity and racism in reproductive health to combat issues impeding effective care. This 4-step framework involves removing power structures, repairing systems, restructuring policies, and addressing pressing concerns within digital health to help combat issues impeding effective care.
Conclusion:
The high rate of diabetic amputations among certain populations is a clear sign that health inequity is still a significant problem in America. However, there are steps that doctors, insurance payors, and patients themselves can take to address this issue.
By expanding access to quality diabetes care, educating patients on how to manage their diabetes, and promoting broader societal changes to reduce health inequity, we can prevent diabetic amputations and improve overall health outcomes for all patients, regardless of their income, race, or background.
It is only by working together that the healthcare community can effectively address these challenges and promote health equity for all. It’s important to recognize that health is more than just medical care. Furthermore, it means investing in creating equitable environments that support healthy living for everyone. Understanding SDoH is the first step in acknowledging the need for such structural changes.
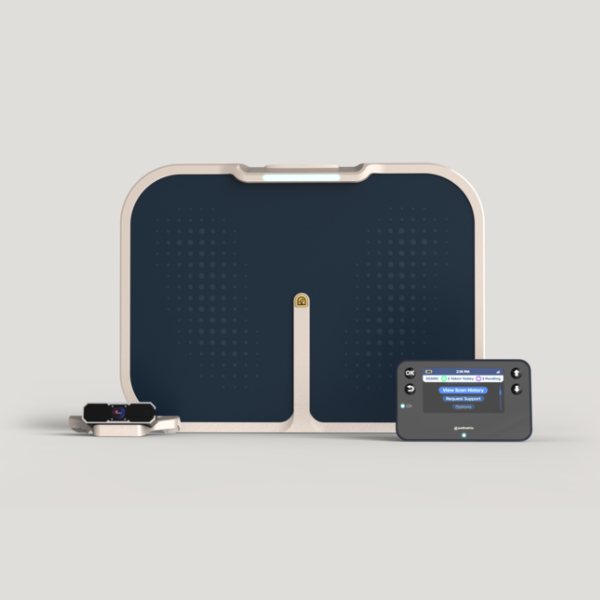
The Podimetrics eBook, “The Big Diabetes Complication That’s Flying Under the Radar,” covers the far-reaching impact of diabetic foot complications. It also discusses the importance of preventing unnecessary amputations and the impact of SDoH.