There is no question that living with diabetes can be challenging and burdensome at times, especially if you’re at risk for diabetic foot ulcers and amputation. The idea of losing a limb to diabetes can be incredibly shocking, scary, and distressing, which means it’s more important than ever to manage your condition as best as possible and reduce your risk.
According to a study in the Journal of Diabetes and its Complications, those who experience diabetic foot ulcers (DFUs) and amputation tend to have higher rates of depression, emotional suffering, social isolation, and reduced quality of life. Awareness of these effects and learning how to cope may help you achieve greater well-being while reducing the risk of future complications.
Here’s a closer look at diabetes distress and strategies to help manage it.
What Is Diabetes Distress?
The CDC defines diabetes distress as the emotional burden that can come with managing diabetes care. For example, if you experience a complication like a foot ulcer or learn you’re at risk for amputation, it’s natural to feel discouraged or overwhelmed, especially when it happens despite your efforts to stay healthy. You may question whether you’re managing your condition as well as you could or feel uncertain about what more you can do to protect your health.
It’s also common for these challenges to impact your emotions in other ways. Feelings of grief, self-doubt, or frustration may arise, which can affect your confidence and sense of well-being. Experiencing these emotions is completely normal and acknowledging them is an important step toward healing.
Remember, diabetes distress doesn’t mean you’ve failed. These feelings are a natural part of facing a complex condition, and there are healthy ways to cope. By addressing them, you can build resilience and take positive steps that empower you to reduce the risk of future complications.
Which Mental Challenges Are Linked to Diabetic Amputation?
Living with or being at risk for diabetic amputation can bring about mental health challenges like depression, anxiety, and post-traumatic stress disorder (PTSD). For many, these feelings may begin when ulcers are first detected and can become more intense as the condition progresses.
A study published in the Journal of Diabetes and Its Complications highlights that emotions such as frustration, sadness, and feelings of powerlessness or social isolation are common experiences for individuals facing amputation. Concerns about body image, including feelings of shame or self-consciousness, can also arise.
These emotional challenges are valid and understandable. Recognizing them is an important step toward seeking support and finding ways to navigate them. Remember, reaching out for help and learning coping strategies can make a meaningful difference in managing these feelings and improving your overall well-being.
Depression
Major depressive disorder is experienced by 21% to 35% of individuals who undergo diabetic amputation, according to a study in the Journal of Yeungnam Medical Science. Factors such as changes in physical function and feelings of helplessness can contribute to this. Depression may also make it harder to engage in rehabilitation and adjust to life after amputation.
Recognizing the emotional impact of this experience is an important step in addressing it. With the right support and care, it’s possible to navigate these feelings and work toward improved well-being and a fulfilling post-amputation life.
Anxiety
It’s natural to experience anxiety after a diabetic amputation, especially as you adjust to life after the loss of a limb. This anxiety may arise as you process the physical and emotional effects of amputation and the changes it brings. Factors like the discomfort of treatments, navigating unfamiliar hospital settings, and uncertainty about the future can add to these feelings.
PTSD
While less than 5% of people who experience diabetic amputation develop post-traumatic stress disorder (PTSD), it’s understandable that the emotional impact of this major change can lead to feelings of intense fear and helplessness. A study published in The Primary Care Companion To the Journal of Clinical Psychiatry suggests that routine screening for both PTSD and depression during follow-up visits can help ensure that everyone who undergoes diabetic amputation receives the emotional support they need.
Strategies for Managing and Reducing Diabetes Distress
Living with a chronic condition like diabetes can be an emotional roller coaster at times—especially when amputation is a real, legitimate risk. However, being honest about your condition and creating realistic goals can help your recovery.
Consider these strategies for reducing diabetes stress and for coping with complications, including diabetic foot ulcers and amputation.
Consider Talk Therapy
Individual or group therapy may help if you and your loved ones are having difficulty adapting to life after amputation. Therapy can help you identify and change negative thought processes and behaviors surrounding your condition. It may also help you develop effective coping skills for grief, depression, anxiety, and PTSD.
Join a Support Group
Support groups exist for people who are living with diabetes and for those who have experienced diabetic amputation. Attending support group meetings can help you feel less alone and isolated. It can also help you pick up new coping skills and tips for adjusting to life after losing a limb.
Take It One Day At a Time
Your daily to-do list may seem overwhelming during the early days of recovery. Pace yourself and be patient, knowing it may take some time for you to get used to doing certain activities after amputation. Go easy on yourself, work on one task at a time, and accept help from friends and family when offered.
Practice Self-Care
Practicing good self-care is essential to maintaining your mental and physical health after amputation and can help you take back your life. Eat healthy foods, get plenty of sleep, spend quality time with loved ones, and set aside time to do your favorite activities. These healthy behaviors can work wonders for your general well-being.
Stay In Contact With Your Healthcare Provider
Your healthcare provider can be a great source of support throughout recovery. Attend all follow-up appointments, and don’t hesitate to mention any concerns you may have about your physical or mental health.
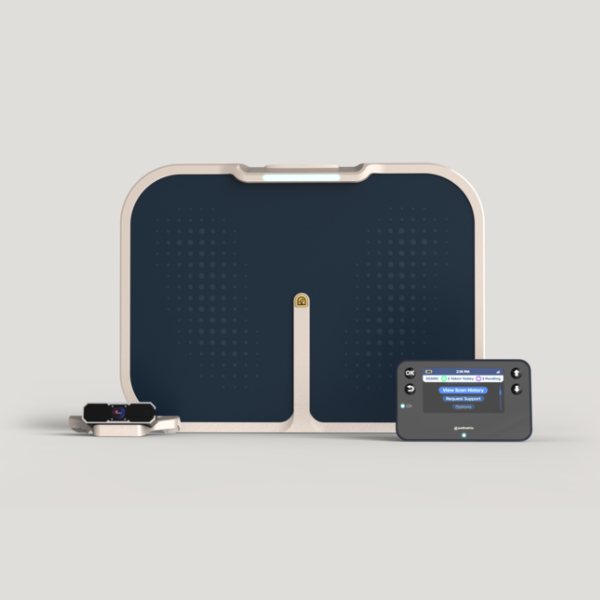
Consider asking your provider about additional resources for diabetes self-care, including diabetes self-management education and support (DSMES) and remote temperature monitoring (RTM). DSMES provides personalized services for diabetes management, especially in instances where factors like health equity and social determinants of health put you at greater risk for ulcers and amputation. RTM uses technology that allows your provider to remotely monitor the temperature of your feet to identify and treat ulcers early on.
Visit our Patient Resources page to learn more about RTM using the Podimetrics SmartMat™ Program, and how it can help reduce your risk for future or repeat amputation.