Diabetes affects nearly 12% of the U.S. population and is concerningly more prevalent in underserved populations—particularly racial and ethnic minority groups and those with low socioeconomic status. For instance, the risk for developing diabetes is 50% greater in Hispanic and African American people than in other groups and three times greater among people who earn less than $80k a year.
Gaps in health equity, such as those mentioned above, impact providers, patients, and employers alike. Remote temperature monitoring (RTM) is a solution that can help address challenges for all parties and help millions of people with diabetes become healthier and reduce their risk for amputation.
Read on to learn more about RTM’s benefits for underserved populations and how this solution can help close the health equity gaps impacting the risk of diabetes-related amputations.
What Is Remote Temperature Monitoring (RTM)?
RTM refers to having a healthcare provider monitor the feet’s temperature remotely. Thermometry plays a vital role in diabetes foot care, as it can help determine whether someone with diabetes is at risk for diabetic foot ulcers and amputation.
With RTM, a provider reviews temperature readings and intervenes if an issue arises. More specifically, a provider looks for signs of inflammation—a hot spot that develops before a foot ulcer forms—in one or both feet. Inflammation can indicate tissue breakdown, which may develop into diabetic foot ulcers if not monitored and treated by a healthcare provider.
When noticeable temperature differences are detected, a provider can work with a patient to modify the treatment plan and lifestyle to help control inflammation. This technology can pave the way to early intervention, improved overall health, and prevention of diabetic amputation.
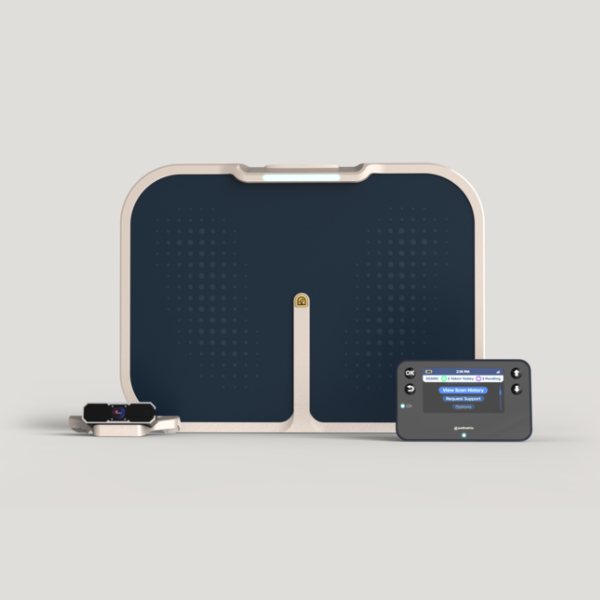
An example of RTM is the Podimetrics SmartMat™ Program —an advanced remote foot monitoring solution designed to help track patients’ foot health daily. Patients step on the SmartMat for just 20 seconds each day, and the Podimetrics team monitors for early signs of inflammation that could lead to diabetic foot complications like foot ulcers. If an issue arises, patients receive personal guidance and, if needed, Podimetrics can help alert the provider for further intervention.
What Are Health Disparities In Diabetic Foot Care?
Many health disparities that affect diabetic foot care fall under the domains that make up social determinants of health (SDoH). SDoH refers to the conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect their health, functioning, and quality of life. Addressing SDoH in diabetes is an important first step to achieving health equity for people living with this chronic condition.
For example, low income and lack of transportation contribute to health disparities in diabetes care. These factors can often prevent people from receiving quality care, especially those living in rural areas.
Limited access to healthy foods is another major health disparity in diabetes, given how certain foods may contribute to diabetes or protect against the disease. According to a study in Diabetes Care, the prevalence and risk for type 2 diabetes is generally higher among people who live in neighborhoods where fast-food restaurants and convenience stores are widely available. Ultra-processed foods, including fast foods, are known to drive inflammation, which in turn increases the risk of foot ulcers and amputation in people living with diabetes.
How Can RTM Address SDoH and Make Preventive Care More Accessible?
Foot checks at home are one of the most effective ways to prevent lower-limb amputations in diabetes, reports the CDC. RTM shouldn’t replace daily foot checks but provides an additional layer of support with the potential to address nearly every SDoH factor and disparity that contributes to the health equity gap in diabetic foot care.
Here’s a look at how RTM can make preventive care more accessible to those with complex diabetes who face SDoH-related challenges:
- RTM is relatively easy to use. It can help patients learn more about their condition and reduce their risk for complications such as diabetic foot ulcers. It provides patients with an added layer of support and accessible care from the comfort of their homes.
- RTM may reduce travel needs to and from the clinic. This remote technology can reduce the number of trips to and from patients’ healthcare providers, saving lots of time and money—especially for those living in rural areas.
- RTM can help providers spot issues early on. This allows for early treatment and prevention of diabetes-related complications, including foot ulcers and diabetes-related amputation.
- RTM is fast and convenient. Many of the technologies used in RTM take up very little time in the patients’ day, which can be highly convenient for those who lack enough time in their schedules to visit their providers on behalf of factors like work and childcare.
- RTM comes with high-quality care. Access to quality health care is a major health disparity among underserved populations. With RTM technologies like the SmartMat, support teams can guide patients on how to address any issues.
RTM offers a countless number of benefits for employers, given how early detection and treatment of foot ulcers in those with diabetes may lead to higher retention and productivity in the workplace. This innovative tech can even lead to massive savings for health plans, given it reduces the need for hospitalization and surgical procedures such as amputation.
RTM has the potential to significantly increase access to care for underserved populations and those affected by health equity and SDoH. Visit our Patient Resources page to learn more about RTM and the Podimetrics SmartMat™ Program.